3 Symptoms Suggesting A Rotator Cuff Tear
If you are over 30 years old, chances are greater than 30% at one time or another you have experienced some type of shoulder discomfort. All human beings can relate to whether it was a transient sting in the shoulder after a sudden tug or fall, or a lingering nagging ache that just does not seem to go away.
You don’t have to be an athlete to experience shoulder pain. Second to back pain, shoulder pain is the most common musculoskeletal problem seen by health care professionals in this country. More than 6 million patients seek medical care for shoulder pain in the U.S. each year. More than 30% of these are related to the rotator cuff, and approximately 1 in 7 of rotator cuff issues eventually undergo surgery.
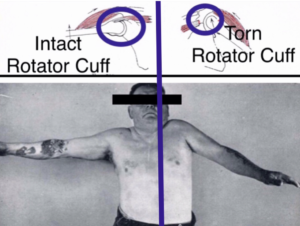
This high prevalence of shoulder pain, and particularly, rotator cuff disease lies in the unique anatomy of our shoulder joints as being the most mobile joint in our body. This mobility gives us our ability to place our hands virtually anywhere in space, such as reaching for that grocery bag in the back seat of a car or screwing in that high ceiling light bulb. In exchange for this increased mobility comes with it inherent instability. 100% of shoulder stability rely on the rotator cuff muscles. There is no bony socket for structural support as in the hip joint. The 4 rotator cuff muscles emanate from the shoulder blade (scapula) and extend out toward the top of the arm bone (humerus) like a group of outcropping legs of an octopus. These are the 4 rotator cuff tendons. These tendons are supple to allow directional changes when the arm moves, however must be simultaneously stiffen up to keep the shoulder joint centered and aligned during arm motion and prevent dislocation. It is this delicate balance between flexibility and rigidity that is so taxing on the rotator cuff.
Rotator cuff disease present in various shades of gray. This can be construed as the fabric of your jeans where they go through varying degrees of wear and tear. These may range from a simple surface discoloration, to mild fraying, to small separation, all the way to a large gap. The actual tears may be either acute or acute-on-chronic or most commonly may develop as a result of a chronic degeneration process. In fact, an estimated 50% of healthy population have radiographic evidence of bilateral rotator cuff tears after age 66 years, although symptoms may vary. It is noted that statistically, almost all full thickness rotator cuff tears occur in individuals over 40 years of age. Full thickness rotator cuff tears in younger individuals are invariably associated with a catastrophic event that leaves no guess work whether the tendon is torn or not.
The 3 most common complaints by patients who have full thickness rotator cuff tears are : (1) Pain at night and unable to sleep on the affected side. (2) History of recurrent episodes of shoulder “tendinitis” or “bursitis”. These episodes of shoulder soreness may seem to have gone away after a period of rest, or use of anti inflammatory medication, or even a cortisone injection. But these episodes become more frequent and linger longer in spite of rest and medication. (3) Reproducible pain and weakness with arm elevations overhead or against resistance, particularly painful when the arm externally rotates such as when trying to put the arm into the sleeve of a jacket.
Treatments are varied. Not everyone with rotator cuff tears necessarily undergo surgery. Many factors come into the decision making process. Most importantly being how much does the shoulder bother you? How frequent, how severe, and under what circumstances? How much are you willing to live with the symptoms and how much are you willing to change your activity in exchange for less of symptoms? How is your health in general and are you willing to accept the potential risks and complications associated with surgery? Keeping in mind that there may be a need for repeat surgery in the event that the repair does not heal. What are your goals and expectations? Surgery is no panacea and treatment options can only be arrived after thorough discussions with your treating surgeon. Everyone is treated differently. Individual variations must be kept in mind.
In spite of technological advances and improved surgical techniques, unfortunately 10-90% of all rotator cuff repairs fail to heal after surgery. This has to do with the biology of healing. Broken bones reliably heal, because it is bone-to-bone healing. Torn muscles heal, because it is muscle-to-muscle healing when sewn together. Even in circumstances where tendons are torn in mid substance such as sewing back the torn achilles tendon, tendon-to-tendon, they heal. But in the case of the rotator cuff tendon, where the tendon is detached from the bone, when repaired together, it is relying on tendon-to-bone healing. Tendon-to-bone healing is not very reliable because tendon and bone are two dissimilar substances. Just like oil and vinegar, they are difficult to mix. However, remarkably, 60-85% of those with rotator cuff tears seem to have successful outcomes after non-operative management. In fact, as an entire population, over 95% of those individuals with full thickness rotator cuff tears over age 65 never wind up having surgery.
In summary, it is not the end of the world when you are diagnosed to have a rotator cuff tear. It all depends on your goals and expectations. Chances are overwhelmingly in your favor for a good outcome provided you have a good understanding of yourself, whether you choose surgery or not. Most importantly, the essential common denominator, whether surgery or no surgery is proper rotator cuff management, rehabilitation, and strengthening. Yes, a shoulder may be strengthened even in light of a rotator cuff tear (but obviously only to a certain degree). Any questions may be directed to Dr. Win Chang, Board Certified Orthopaedic Surgeon shoulder specialist, via contact at https://www.shouldersphere.com/.